NHS Continuing Healthcare Procedure
1. The National Framework
The National Framework for NHS Continuing Healthcare and NHS-funded Nursing Care is a document that sets out:
- The principles and legislative context of NHS Continuing Healthcare; and
- The processes of applying for and making a decision about NHS Continuing Healthcare eligibility.
All practitioners must have regard for the framework when carrying out any action in relation to NHS Continuing Healthcare.
Click here to access the National Framework for NHS Continuing Healthcare and NHS-funded Nursing Care.
2. An Introduction to NHS Continuing Healthcare Funding
Defining NHS Continuing Healthcare
NHS Continuing Healthcare (sometimes called fully funded NHS care) is care outside of hospital that is arranged and funded entirely by the NHS.
NHS Continuing Healthcare can be provided in any setting, including:
- A care home;
- A hospice; or
- The person's own home.
Where NHS Continuing Healthcare is provided the NHS must fund all of the services and support that the person requires to meet both their:
- Health needs; and
- Associated Care and Support needs; which includes
- Accommodation related costs of a care home.
If a person receiving Care and Support from the Local Authority under the Care Act is found to be eligible for NHS Continuing Healthcare all legal responsibilities for arranging, funding and reviewing their care transfer to the NHS.
Eligibility for NHS Continuing Healthcare
NHS Continuing Healthcare is only available for people:
- From the age of 18; who
- Need ongoing healthcare as a result of disability, accident or illness; and
- Have a 'Primary Health need', as determined by a comprehensive eligibility assessment process (as set out in the Framework).
The process normally commences with completion of the NHS Continuing Healthcare Checklist by a health or social care professional, although there are circumstances when the checklist does not need to be completed. In all cases, it is the local Integrated Care Board (ICB) that must determine if a person is eligible for NHS Continuing Healthcare.
Primary Health need
This is the threshold that must be met in order for a person to be found eligible for NHS Continuing Healthcare.
Under the Framework a Primary Health need exists if, having taken into account all of a person's needs, it can be said that the main aspects or majority part of the care they require is focused on addressing and/or preventing health needs.
It is the responsibility of a multidisciplinary team to recommend to the ICB whether or not the threshold is met.
Personal health budgets
If a person receives NHS Continuing Healthcare they should be provided with a Personal Health Budget, in much the same way as they would be provided with a Personal Budget if the Local Authority were meeting their needs.
The allocated health professional should then plan with the person how best to use this budget to meet their needs, which could include through a Direct Payment. This process is similar to Care and Support Planning in adult social care.
For further information about personal health budgets see: NHS, What is a personal health budget?
3. Roles and Responsibilities
The role of Case Managers
Through any assessment or review process practitioners should:
- Identify when a person may be eligible for NHS Continuing Healthcare; and
- Provide information to the person (and their family) about NHS Continuing Healthcare (whenever it is requested or would be beneficial); and
- Seek the person's consent to complete the NHS Continuing Healthcare checklist (of if they lack capacity decide whether it is in their Best Interests to continue); and
- Complete the NHS Continuing Healthcare checklist; or
- Make a referral to the Complex Care Team for a Checklist to be completed.
Guidance about when a referral to the Complex Care Team for a Checklist is required, and how to refer to the team can be found in the 'Continuing Healthcare Checklists and FNC Processes' document in the Local Resource area by clicking here.
The role of the Complex Care Team
The Complex Care Team is part of the Integrated Services Complex Care Hub. The Hub also comprises of the Swindon ICB Continuing Healthcare Team, who are ultimately responsible for funding decisions.
The Complex Care Team will either;
- Quality assure any Checklist submitted by a Local Authority team; or
- Complete a Checklist following a referral from a Local Authority team.
The team may also case manage complex cases that may or may not be in receipt of health funding.
When quality assured and reviewed the Complex Care Team will submit the Checklist to the ICB Continuing Healthcare Team at the hub where a decision will then be made about the need for a full assessment of eligibility.
If a full assessment is required the Integrated Services Complex Care Hub must appoint a suitably qualified practitioner to coordinate the process set out in the Framework. This could be a professional from the Complex Care Team, or a professional from the ICB Continuing Healthcare Team.
Regardless of whether or not they act as the coordinating practitioner a professional from the Complex Care Team will always be a part of the multidisciplinary team completing the Decision Support Tool (DST).
If NHS Continuing Healthcare is awarded, the team will take steps to transfer Local Authority funded services and support to the health professional that will be assuming care management responsibilities.
The role of the coordinating practitioner
The practitioner appointed by the Integrated Services Complex Care Hub to coordinate the process set out in the framework should;
- Explain the NHS Continuing Healthcare assessment process to the person (and/or their representative);
- Decide who should be part of, and establish the multidisciplinary team;
- Ensure the process is completed in a timely way;
- Present the recommendation of the multidisciplinary team to the ICB; and
- Notify the person (and/or their representative) and the Local Authority of the ICB's decision.
Note: Under the Framework the coordinator may also assume a role as part of the multidisciplinary team if they deem this to be appropriate.
The role of the Integrated Care Board
After the assessment process is completed and the multidisciplinary team has made their recommendation the ICB must then make a decision about whether or not the person is eligible for NHS Continuing Healthcare.
If a full assessment of eligibility is carried out and the person is deemed not eligible for NHS Continuing Healthcare the ICB should consider whether the person may be eligible for either NHS-funded Nursing Care or a joint package of health and social care.
If a full assessment of eligibility for NHS Continuing Healthcare is not required the ICB should still consider whether the person may be eligible for NHS-funded Nursing Care.
Maximising participation of the person
A core value and principle of the Framework is to ensure the involvement and participation of the person at all stages of the process, from completing the checklist to the point where a decision is made about eligibility and beyond.
As a minimum the MDT should;
- Ensure that the person and/or their representative is fully and directly involved in the process and any decision making (to the extent that it is possible to do so);
- Take full account of the person's own views and wishes, ensuring that their perspective is the starting point of every part of the process;
- Address communication and language needs;
- Seek consent to assessment and sharing of records;
- Deal openly with issues of risk; and
- Keep the person (and/or their representative) fully informed.
Under the Framework, if a person with the relevant capacity refuses to participate in the assessment process, the Multi-Disciplinary Team (MDT) may consider relevant health and care records or existing assessments to determine the best way to meet their needs and whether they are eligible for NHS Continuing Healthcare. The consequences of undertaking the NHS Continuing Healthcare assessment as a paper-based exercise should be carefully explained to the person, including that this may affect the quality of the assessment, for example if the health and care records to be considered by the MDT are not up-to-date or accurate.
Practitioner skills and knowledge
The Framework requires that practitioners involved in the process have received the necessary training to fulfil their role and meet their responsibilities.
You should speak with a line manager if you are concerned about your skills or knowledge around the NHS Continuing Healthcare framework.4. Identifying when a Person may be Eligible
Why it is important to identify possible eligibility
As a social care practitioner it is important that you understand when a person may be eligible for NHS Continuing Healthcare, for both person centred and statutory reasons. There are also very significant financial consequences for the person and their family as NHS Continuing Healthcare is provided free of charge whereas Care and Support provided by a Local Authority is means-tested and can involve substantial charges.
Person centred benefits
It is unlikely that practitioners based in the Local Authority will:
- Understand how best to meet complex health needs; or
- Have access to appropriate services to meet the needs.
Statutory implications
Under section 9 of the Care Act where it appears that a person may be eligible for NHS Continuing Healthcare the Local Authority must refer them to the ICB.
In addition to this requirement under section 22 of the Care Act the Local Authority is not permitted to provide services and support to people when it is the legal duty of the NHS to provide them unless;
- The support being provided is merely incidental or ancillary (secondary) to doing something else to meet Care and Support needs; or
- The support is of a nature that the Local Authority could be expected to provide.
The result of this can be that some of the person’s needs may go unmet if suitable NHS provision is not made.
People that may be eligible
It is important that no assumptions or generalisations are made about a person's possible eligibility for NHS Continuing Healthcare. However, where a person’s needs appear to include significant health needs, they may be eligible, and steps should be taken to consider eligibility.
If you are not sure of a person's possible eligibility you should seek the support and advice of your line manager.
When you have identified that a person may be eligible for NHS Continuing Healthcare you should:
- Provide information to them (or their representative) about NHS Continuing Healthcare; and
- Seek their consent to complete the NHS Continuing Healthcare checklist; and
- Complete the checklist to determine whether a referral for a full assessment of eligibility by the ICB is indicated.
Guidance on each of these steps can be found below.
5. Providing Information and Advice about NHS Continuing Healthcare
You are expected to be able to provide accessible information and advice about NHS Continuing Healthcare whenever:
- A person/carer asks for it; or
- You have identified that a person may be eligible.
The following is a list of the information that you should be able to provide:
- What NHS Continuing Healthcare is;
- What factors might make a person eligible for NHS Continuing Healthcare;
- The process of completing a NHS Continuing Healthcare checklist;
- What happens following the checklist;
- Who is responsible for making decisions about eligibility;
- How decisions about eligibility are made;
- The implications of an 'eligible' decision; and
- The implications of an 'ineligible' decision.
It is important when providing information about NHS Continuing Healthcare you make clear the checklist is not a determination of eligibility, nor is it a guarantee that a full assessment will be carried out.
The Department of Health and Social Care has published a Public Information Leaflet that can be provided.
If the person who is requesting information (or for whom it would be beneficial) is a person with a learning disability the NHS has produced easy read information that can be given to them. See: NHS care for people with long term health needs.
You should speak with a line manager if you are concerned about your skills or knowledge around the NHS Continuing Healthcare framework before providing advice about it.
6. Consent
Seeking consent
Under the Framework, the consent of the person is not required before completing a NHS Continuing Healthcare Checklist or making a referral to the ICB. However, this does not mean that it should not be sought.
Consent should be sought to:
- Complete the Checklist; and
- Provide a copy of the Checklist to the ICB; and
- If positive, make a referral for full assessment by the ICB.
Consent should be:
- Explicit;
- Specific;
- Informed; and
- Freely given.
If the person refuses to give consent, or if consent cannot be sought (for example the person is unconscious), then a checklist should still be completed and, if positive, a referral made to the ICB.
The nature of the consent given (or not given) must be clearly recorded on:
- The person's file;
- The checklist; and
- Where required, the referral.
For further information about consent please refer to the Framework.
Mental capacity and consent
If you believe that the person may lack capacity to consent this must be formally established through a proportionate Mental Capacity assessment.
If a person who lacks capacity to consent has a Lasting Power or Attorney or Deputy with the relevant authority, they should be consulted about the matter. However, regardless of their view, if the local authority deems it to be in the person's best interests, the checklist should still be completed and, if positive, a referral made to the ICB.
Information and practice guidance regarding the requirements and processes of mental capacity assessment and Best Interests decision making can be accessed in the Mental Capacity Act 2005 Resource and Practice Toolkit.
7. Completing the NHS Continuing Healthcare Checklist
Using this section of the procedure
This section of the procedure should be used by all practitioners with responsibility for completing the Checklist, including care managers and the Complex Care Team.
Guidance about when a Checklist should be completed by the Complex Care Team can be found in the 'Continuing Healthcare Checklists and FNC Processes' document in the Local Resource area by clicking here.
The person completing the NHS Continuing Healthcare checklist
The person completing the NHS Continuing Healthcare checklist must be trained in its use and familiar with the NHS Continuing Healthcare framework.
You should speak with a line manager if you are concerned about your skills or knowledge around the NHS Continuing Healthcare framework before completing the NHS Continuing Healthcare checklist.Advocacy
Under the Framework it is important to maximise the participation of the person in all parts of the process, including the Checklist stage. The minimal requirements of the Framework are explained above in section 3 of this procedure.
You should establish whether the person wishes to have (or needs) representation. If so you should:
- Consider whether there is a family member or friend able to represent them; and
- If not, arrange advocacy support whenever time allows.
People that should be present when the checklist is completed
When the checklist is completed the following people should be present:
- The person; and
- Any representative or advocate.
No other person is required to be present, but it is usual for any informal carers to be consulted. If you feel it would be beneficial to consult with somebody else you may do so, as long as:
- The person consents to their involvement; or
- The person lacks capacity and a decision is made in their Best Interests.
The NHS Continuing Healthcare checklist
The NHS Continuing Healthcare checklist can be printed, e-mailed and saved as required.
Deciding the level of need
The NHS Continuing Healthcare checklist is divided into 11 sections, covering each of the 11 static care domains of the framework. These are:
- Breathing;
- Nutrition;
- Continence;
- Skin Integrity;
- Mobility;
- Communication;
- Psychological/Emotional;
- Cognition;
- Behaviour;
- Drug therapies and medication (symptom control); and
- Altered states of consciousness.
Each section contains a range of statements (A, B or C), similar to the example below (which is a replica of the Breathing section of the checklist);
| C | B | A | |
| Breathing* | Normal breathing, no issues with shortness of breath. OR Shortness of breath or a condition, which may require the use of inhalers or a nebuliser and has no impact on daily living activities. OR Episodes of breathlessness that readily respond to management and have no impact on daily living activities. |
Shortness of breath or a condition, which may require the use of inhalers or a nebuliser and limit some daily living activities. OR Episodes of breathlessness that do not consistently respond to management and limit some daily activities. OR Requires any of the following:
other therapeutic appliances to maintain airflow where individual can still spontaneously breathe e.g. CPAP (Continuous Positive Airways Pressure) to manage obstructive apnoea during sleep. |
Is able to breathe independently through a tracheotomy that they can manage themselves, or with the support of carers or care workers. OR Breathlessness due to a condition which is not responding to therapeutic treatment and limits all daily living activities. OR A condition that requires management by a non-invasive device to both stimulate and maintain breathing (non-invasive positive airway pressure, or non-invasive ventilation) |
| Brief description of need and source of evidence to support the chosen level | Write A, B or C below: | ||
You must:
- Circle or highlight the individual statement that best matches the needs of the person; and
- Write the corresponding letter (either A, B or C) in the box; and
- Provide a brief and concise summary of the person's needs in that domain and the evidence upon which you have based your judgement.
Where the Checklist is completed by a practitioner outside of the Complex Care Team copies of the evidence used do not have to be provided but the manner in which you reference the evidence on the Checklist should make it easy for the Complex Care Team to locate if required.
If you are of the view that the person's needs are likely to increase in the next 3 months, this should be reflected by the statement that you select.
The equality monitoring data form
The equality monitoring data form at the end of the checklist should be completed by the person, with your support as required. This form must be submitted to the ICB with the other areas of the checklist.
Deciding whether a full assessment request should be made
When you have circled a statement in each of the care domains you must record the total number of A's, B's and C's selected.
At this point any Checklist completed outside of the Complex Care Team should be submitted to the Complex Care Team for quality assurance and review.
Send the Checklist using ComplexCare@swindon.gov.uk.
As part of quality assurance and review the Complex Care Team will determine whether or not a request for a full assessment should be made to the ICB Continuing Healthcare Team.
A referral for a full eligibility assessment must always be made when there are:
- 2 or more domains selected in column A; or
- 5 or more domains selected in column B, or 1 selected in A and 4 in B; or
- 1 domain selected in column A where the domain has an asterisk with any number of selections in the other 2 columns.
If the above does not apply it may still be appropriate for a full assessment to be carried out if the overall level of need is deemed to be complex, intense or unpredictable in nature.
Recording the outcome (Complex Care Team)
There are 2 statements at the end of the checklist, one of which must be circled:
- Referral for full assessment for NHS Continuing Healthcare is necessary (known in the Framework as a 'positive' Checklist); or
- No referral for full assessment for NHS Continuing Healthcare is necessary (known as a 'negative' Checklist).
The rational for the decision should be clearly recorded, especially if the threshold upon which a referral must be made has not been met.
When the checklist is complete you must sign and date where specified, and make a record of your contact details.
A record of the outcome, and the rational should also be recorded on the person's electronic file.
Notifying the person of the outcome
The practitioner that completed the Checklist should notify the person of the outcome, specifically:
- Whether a referral to the ICB Continuing Healthcare Team for a full assessment is required; or
- Whether a referral is not required;
- The rational for the decision; and
- Information about how the person (or their representative) can request that the ICB review the decision.
Reviewing the decision
All requests to review NHS Continuing Healthcare decisions must be made to the ICB Continuing Healthcare Team, even if it was the decision of the Complex Care Team not to make a referral.
It is therefore best practice that if a decision is made not to refer, a copy of the checklist is still provided to the ICB Continuing Healthcare Team, so that it is available should the person decide to complain.
Providing copies of the checklist
The person (and any representative) should be provided with a copy of the checklist, regardless of whether a request for a full assessment is to be made.
If a request is to be made to the ICB Continuing Healthcare Team the original checklist should be sent, and a copy should be stored on the person's Local Authority file.
Where a decision is made not to request a full assessment the original checklist should be stored on the person's Local Authority file, and a copy provided to the ICB Continuing Healthcare Team, so that they are aware that NHS Continuing Healthcare has been considered and are able to respond to any complaint that may be made.
8. Requesting a Full Assessment (Complex Care Team)
Secure and timely requests
When a decision is made to request a full assessment of eligibility it is essential that the checklist is sent to the ICB Continuing Healthcare Team in a secure and timely manner to:
- Ensure confidentiality; and
- Avoid any delays in establishing and providing NHS Continuing Healthcare (or any other health funding provision).
The process for making a request
Requests to the ICB Continuing Healthcare Team should be made in line with local processes and requirements.
Providing evidence
Copies of the evidence used do not have to be provided but the manner in which the evidence is referenced on the Checklist should make it easy for the ICB Continuing Healthcare Team and/or any assessor to locate if required.
Making a record
You must record the following on the person's electronic file:
- The date that the request was made; and
- When known, the outcome of the request.
Notification of the outcome
The ICB is expected to make a final decision about eligibility for NHS Continuing Healthcare within 28 days of receiving the request (or sooner if it is more urgent) unless their reasons for not doing so are both:
- Valid; and
- Unavoidable.
The need to carry out a full assessment should therefore be established soon after the Checklist has been provided to them.
It is the ICB's responsibility to notify the person of the outcome of the referral in writing, and advise them of any action they can take if they are not happy with the decision.
The outcome of the referral will be either:
- A full assessment of eligibility for NHS Continuing Healthcare will be carried out; or
- A full assessment of eligibility for NHS Continuing Healthcare will not be carried out.
If a full assessment is to be completed
If a full assessment is to be completed the Integrated Services Complex Care Hub must appoint a practitioner to coordinate the assessment process.
This could be a professional from the Complex Care Team, or a professional from the ICB Continuing Healthcare Team.
Regardless of whether or not they act as the coordinating practitioner a professional from the Complex Care Team will always be a part of the multidisciplinary team completing the Decision Support Tool (DST).
Click here to access the guidance about being part of the multidisciplinary team.
If a full assessment is not required
If the ICB decides that a full assessment to determine eligibility for NHS Continuing Healthcare is not required you should take steps to ensure that the person continues to access Local Authority support and services under the Care Act.
However, if the person lives in a nursing home (or will be moving to one) you should ask the ICB to consider whether or not they may be eligible for NHS-funded Nursing Care (FNC), if the ICB has not already done so.Complaints and requests to review the decision
If the person (or their representative) is unhappy with the decision of the ICB they should complain about it directly to the ICB, and the ICB is required to review their decision.
The Local Authority is not able to manage any complaints relating NHS Continuing Healthcare.
If you are concerned about the decision of the ICB you should discuss any action that may (or may not) be needed to challenge the decision with your line manager.9. The Provision of Relevant Information
If the ICB consults with you as part of the NHS Continuing Healthcare process you must, as far as is reasonably practicable provide any evidence and assistance requested within a reasonable timeframe.
Note: Under the Framework, if a needs assessment under the Care Act 2014 has already been carried out by the local authority and is still relevant to a person's current needs then, in accordance with the relevant regulations, the local authority must use this assessment to provide advice and assistance to the ICB.
Consent to share information
Where the person has relevant capacity, their explicit consent is required for the sharing of personal data with third parties other than health or social care professionals (for example family, friends, advocates, and/or other representatives). It must be made clear to them that they can withdraw their consent for the sharing of personal data with third parties other than health and social care professionals at any time; and it is good practice to ensure that the person is still consenting at each stage. It is best practice to keep a written record of consent for the sharing of personal data with third parties.
10. The Multidisciplinary Team and the Decision Support Tool (Complex Care Team)
The role of the multidisciplinary team
The multidisciplinary team (MDT) must consist of at least;
- Two professionals from different healthcare professions; or
- One healthcare professional and one person with responsibility for assessing Care and Support needs under the Care Act.
It is the expectation in the Framework that the MDT should include professionals from both health and social care, who are knowledgeable about the person's needs and, where possible have been recently involved in the assessment, treatment or care of the person.
The MDT is responsible for;
- Carrying out any assessments required (e.g. a needs assessment or a nursing needs assessment);
- Maximising the participation of the person in the process (see below);
- Consulting with the person, their family and any other person deemed relevant to the decision;
- Reviewing all of the information gathered;
- Applying the Decision Support Tool; and
- Making a recommendation to the ICB about eligibility.
Note: The absence of a needs assessment under the Care Act 2014 should not delay an assessment of eligibility for NHS Continuing Healthcare.
Under the Framework the coordinator may also assume a role as part of the multidisciplinary team if they deem this to be appropriate.
Maximising participation of the person
A core value and principle of the Framework is to ensure the involvement and participation of the person at all stages of the process, from completing the checklist to the point where a decision is made about eligibility and beyond.
As a minimum the MDT should:
- Ensure that the person and/or their representative is fully and directly involved in the process and any decision making (to the extent that it is possible to do so);
- Take full account of the person's own views and wishes, ensuring that their perspective is the starting point of every part of the process;
- Address communication and language needs;
- Seek consent to assessment and sharing of records;
- Deal openly with issues of risk; and
- Keep the person (and/or their representative) fully informed.
Practitioner skills and knowledge
The Framework requires that practitioners involved in the process have received the necessary training to fulfil their role and meet their responsibilities.
You should speak with a line manager if you are concerned about your skills or knowledge around the NHS Continuing Healthcare framework.The Decision Support Tool
The Decision Support Tool (DST) is not an assessment of needs in itself, rather it is the mechanism used to bring together all of the evidence gathered during the assessment process so as to clarify needs and then make a collective professional judgement about eligibility for NHS Continuing Healthcare on the basis of a primary health need.
The NHS Continuing Healthcare Decision Support Tool can be printed, e-mailed and saved as required.
The Care Domains
There are 12 care domains set out in the Decision Support Tool which are the same domains as in the Checklist:
- Breathing;
- Nutrition-food and drink;
- Continence;
- Skin and tissue viability;
- Mobility;
- Communication;
- Psychological and emotional needs;
- Cognition;
- Behaviour;
- Drug Therapies and medication (symptom control);
- Altered States of consciousness; and
- Other significant care needs.
In each domain the actual health and social care needs of the person should be described, along with the evidence that has informed this judgement.
Determining health and social care needs
Often it can be difficult to determine which needs are health needs and which are social care needs.
A health need
A 'health need' is described in the Framework as;
- A need related to the treatment, control, management or prevention of a disease, illness, injury or disability; and
- The care or aftercare of a person with these needs (whether or not the tasks involved have to be carried out by a health professional).
Some of the domains in the DST are clearly health needs by nature (breathing, drug therapies, ASC) but the remaining domains are likely to have an element of both health and social care need, and the role of the MDT is to agree whether the nature of the care required indicates a more prominent health or social care need overall.
Social care needs
Under the Framework a 'social care need' is taken to be any need related to the Care Act eligibility criteria:
- Managing and maintaining nutrition;
- Maintaining personal hygiene;
- Managing toilet needs;
- Being able to make use of the home safely;
- Maintaining a habitable home environment;
- Developing and maintaining family or other personal relationships;
- Accessing or engaging in work, training, education or volunteering;
- Making use of necessary facilities or services in the local community; and
- Carrying out any caring responsibilities for a child.
Eligibility criteria a-e clearly overlap with the domains of the DST, whereas the others are all social care needs. It is important to make sure that the needs that do not fit into the DST domains are still included in decision making.
Deciding the level of health need
When all relevant health and social care needs in a care domain have been identified the multidisciplinary team must consider and agree the overall level of health need in each domain, which will be one of the following:
N=No needs
L=Low needs
M=Moderate needs
H=High needs
S=Severe needs
P=Priority needs
This decision should be made having regard for the frequency and intensity of need, unpredictability, deterioration and any instability. Guidance on these characteristics can be found in the table below:
| Nature | 'Nature' is about the characteristics of both the individual's needs and the interventions required to meet those needs. | Questions that may help to consider this include:
|
| Intensity | ‘Intensity’ is about the quantity, severity and continuity of needs. |
Questions that may help to consider this include:
|
| Complexity | 'Complexity' is about the level of skill/knowledge required to address an individual need or the range of needs and the interface between two or more needs. | Questions that may help to consider this include:
|
| Unpredictability | 'Unpredictability' is about the degree to which needs fluctuate and thereby create challenges in managing them. It should be noted that the identification of unpredictable needs does not, of itself, make the needs 'predictable' (i.e. 'predictably unpredictable') and they should therefore be considered as part of this key indicator. | Questions that may help to consider this include:
|
It is important to refer to guidance in the Decision Support Tool when agreeing the level of need in each care domain. This is because:
- The description of P, S, H, M and L varies across care domains; and
- Not all levels of need can be applied to all domains.
The concept of a 'well-managed' need
Well managed needs are those needs that are currently having little or no impact on the person's health or wellbeing because of the positive effects of the support they are receiving.
The Framework is clear that a well managed need is still a need.
The number of recorded incidences of need (e.g. in behaviour) should not be used as the sole factor when determining the overall level of need in the care domain. This could lead to a false level of need being agreed. Instead, the MDT should consider whether other factors are impacting on the incidences of need, for example the environment, and whether changes can be made to these factors that could reduce or eliminate the need.
If the level of health need is not clear
If it is not clear what the level of health need is, or if there is disagreement about this the coordinating practitioner should; make a record of any disagreement or difficulties occurred in reaching the recommendation so that the ICB can discuss this when making a decision about eligibility.
Deciding if there is a Primary Health need
After agreeing the level of health need in each care domain (i.e. P, S, H, M, L or N) the information must be summarised into the following table, which appears on page 39 of the Decision Support Tool:
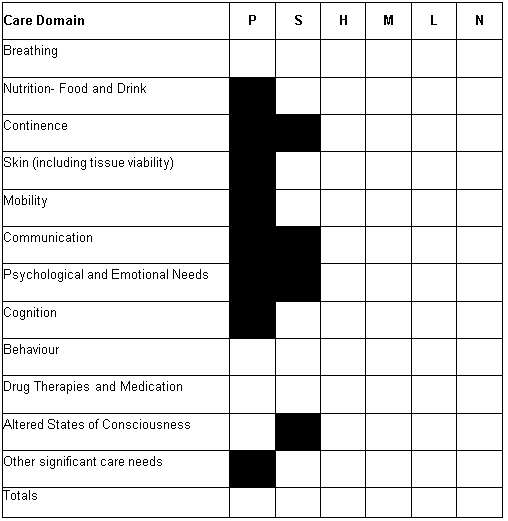
After completing the table the multidisciplinary team must agree whether the total effects of all needs across all domains equates to the existence of a Primary Health need (in which case a recommendation of eligibility for NHS Continuing Healthcare would be made).
Indicators of a Primary Health need
Under the Framework a person is deemed to have a Primary Health need if it can be said that the main aspects or majority part of the care they require is focused on addressing and/or preventing health needs.
A recommendation of eligibility for NHS Continuing Healthcare should normally be made when;
- A Priority level of need is identified in any one of the 4 care domains that carry that level; or
- A total of 2 or more incidences of Severe level of need across any care domains.
In all other cases the multidisciplinary team must to consider the quality and quantity of care in more detail, using the four characteristics of;
- Nature;
- Intensity;
- Complexity; and
- Unpredictability.
Difficulty agreeing a recommendation
If the MDT is having difficulty in establishing an agreed recommendation it is not unusual for it to agree to reconvene a further meeting. This can serve the purpose of gathering additional information to ensure the recommendation is based on the most up to date and relevant information as possible.
If the existence of a primary health need is not clear
If the existence of a primary health need is unclear the coordinating practitioner should:
- Make the recommendation that they believe is most appropriate; but
- Make a record of any disagreement or difficulties occurred in reaching the decision; so that
- The ICB can discuss this when making the final decision about eligibility.
Making the Recommendation
The coordinating practitioner is responsible for notifying the ICB of the multidisciplinary team's recommendation, which will be either:
- That the person is not eligible for NHS Continuing Healthcare (because they do not appear to have a Primary Health need); or
- That the person is eligible for NHS Continuing Healthcare (because they appear to have a Primary Heath need).
If the recommendation is that the person does not have a Primary Health need (and is not eligible for NHS Continuing Healthcare) the coordinating practitioner should recommend whether:
- The person would benefit from on-going health support; and
- If so, whether any joint package of health and social care arrangements may apply; or
- If the person lives in a nursing home (or will be moving to one), whether they may be eligible for NHS-funded Nursing Care (FNC).
If you are concerned about the recommendation made by the coordinating practitioner you should discuss any action that may (or may not) be needed to challenge the recommendation with your line manager.
11. After Eligibility is Determined (Complex Care Team)
Notification of the outcome
The coordinating practitioner is responsible for formally notifying the person of the outcome in writing, explaining the implications of the outcome to them and letting them know how they can make a complaint about the decision.
If the person is eligible
The timeframe for transfer of services from the Local Authority to the ICB should be agreed at the point that a decision about eligibility is made. This should reflect local policy and should allow for:
- Any remaining relevant assessment and planning processes to be carried out by the ICB; and
- Services to be arranged.
During any transfer of services you should work as required with the health professional that will be assuming care management responsibilities to:
- Introduce them to the person (and their family);
- Ensure they have all relevant information about the person's needs (having full regard for consent); and
- Ensure they have all relevant information about the current services and support being provided to the person.
When the transfer of services is completed you should take steps to close the person's case unless there is a need to maintain involvement as part of an on-going safeguarding concern or investigation.
If the person is not eligible
If the person is not eligible for NHS Continuing Healthcare the Local Authority remains legally responsible for meeting eligible needs under the Care Act, which can include support provided by a health professional when:
- It is merely incidental or ancillary (secondary) to doing something else to meet Care and Support needs; or
- It is of a nature that the Local Authority could be expected to provide.
If you believe that the person may be eligible for alternative heath funding provision and that this has not been considered you should discuss this with your line manager in the first instance.
Funded nursing care
If the ICB has agreed that the person is eligible for NHS-funded Nursing Care see the NHS-funded Nursing Care Procedure.
Joint package of health and social care
If the ICB has recommended that a joint package of health and social care should be arranged, see the Joint Packages of Health and Social Care Procedure.
Safeguarding responsibility
Regardless of eligibility for NHS Continuing Healthcare the Local Authority remains legally responsible for:
- Any ongoing adult safeguarding processes or investigations regarding the person; and
- Responding to any new safeguarding concerns that may arise; but
- It is expected that the ICB will have an important role in any new enquiries.
Equipment
If a person is eligible for NHS Continuing Healthcare they will assume responsibility for providing any equipment the person may require. However, where all Occupational Therapy services are commissioned jointly no changes will be required.
Reviewing eligibility
Eligibility/non-eligibility for NHS Continuing Healthcare is not indefinite, as needs can change.
The ICB
The ICB have a statutory responsibility to review the person's services 3 months after the transfer of funding responsibility, and then every 12 months after that. If there is any evidence to suggest that the person may no longer be eligible for NHS Continuing Healthcare a referral may be made to the Local Authority to be part of the multidisciplinary team who considers this once more.
The Local Authority
If the Local Authority believes there to be a change in the person's needs, and that a person who was previously ineligible may now be eligible, a further NHS Continuing Healthcare checklist should be completed as outlined in this procedure.
Complaints and challenges to the decision
Challenges to the decision
If you disagree with any outcome that refuses NHS Continuing Healthcare funding you should discuss any action that may (or may not) be needed to challenge the decision with your line manager. Challenges should be made in line with the local dispute resolution process.
Complaints about the decision
If the person (or their representative) is unhappy with the decision of the ICB they should complain about it directly to the ICB.
In all cases, if the ICB subsequently reverses its decision, it should make arrangements to reimburse the Local Authority for the cost of services that it has provided during that time. Where applicable, any financial contribution made by the person for those services should also be reimbursed.
12. The Responsibility of Meeting Needs
During assessment
Inpatient settings
See Section 13 of this procedure 'NHS Continuing Healthcare in Acute Hospital Settings'.
Other settings
If the Local Authority is already providing services to the person, it remains the legal responsibility of the Local Authority to meet the person's eligible needs until:
- A decision about eligibility for NHS Continuing Healthcare is made; and
- Where eligible, the person's services and support have been transferred to the ICB.
During reassessment
If a person is already receiving support and services through NHS Continuing Healthcare but their eligibility is under review it is the legal responsibility of the ICB to continue meeting the person's needs until:
- A decision about on-going eligibility for NHS Continuing Healthcare is made; and
- Where ineligible, the person's services and support have been transferred to the Local Authority.
Delays in assessment/reassessment
With the exception of referrals made in acute hospital settings arrangements in place at the point of Checklist submission to the ICB Continuing Healthcare Team should remain in place until a determination is made.
In most cases the ICB is expected to make a final decision about eligibility for NHS Continuing Healthcare within 28 days of receiving the referral (or sooner if it is more urgent). In situations where there are valid and unavoidable reasons for doing so, decisions can take longer.
The Local Authority and the ICB should agree arrangements for appropriate reimbursement if a decision is subsequently made that the person is eligible/ineligible for NHS Continuing Healthcare. Where applicable, this should also include reimbursement of any financial contributions made by the person.
Delays in the transfer of services after a determination
The timeframe for transfer of services from the Local Authority to the ICB (or vice versa) should be agreed at the point that a decision about eligibility is made. This should reflect local policy and should allow for:
- Any remaining relevant assessment and planning processes to be carried out; and
- Services to be arranged.
If this process is likely to take some time, or is delayed for any reason that is not valid or unavoidable, the Local Authority and the ICB should agree arrangements for appropriate reimbursement.
The Framework is clear that the person should not experience any gaps in care as a result of delays, regardless of the cause. This means that under no circumstances should either organisation cease to provide services to the person until alternative arrangements are in place.
13. Continuing Healthcare in Acute Hospital Settings
Using this section of the procedure
This section sets out the specific considerations and requirements for social care practitioners when the person who may be eligible for NHS Continuing Healthcare is an in-patient in an acute hospital setting.
When eligibility should be considered
Eligibility should not be considered until;
- All acute or emergency treatment has been completed; and
- The likely outcome of any rehabilitation treatment or therapy is clear; and
- The person's needs upon discharge are clear.
The Framework expects that most assessments for eligibility will not take place until after the person has been discharged from hospital.
In line with the expectation of the Framework Swindon's local policy does not allow for Checklists to be completed in hospital.
Discharging to Assess
When arranging a Discharge to Assess (D2A) bed for someone who will need a Checklist completing a request should be made to the Complex Care Team to make arrangements to complete the Checklist.
This request should be made to ComplexCare@swindon.gov.uk.
The Complex Care Team will make the necessary arrangements to complete the Checklist within 2 weeks of discharge. The ICB is legally responsible for providing all care and treatment to the person in the interim period unless:
- The person was in receipt of a Local Authority funded service prior to admission; and
- The same service is still available; and
- The service does not needs to be altered to meet the person's post discharge needs.
In this case the Framework allows for the ICB to request the Local Authority reinstate and continue funding that service whilst the eligibility assessment takes place.
The Local Authority does not have a duty to do this and before responding to such a request you must be clear about local arrangements that have been agreed between the Local Authority and the ICB. In the event of a dispute, the local dispute resolution procedure should be followed.
Where the Local Authority agrees to reinstate services and the ICB subsequently decides that the person is eligible the Local Authority must be reimbursed for all care costs from the date of discharge. Where applicable, any financial contribution made by the person should also be reimbursed.
14. Fast Track Pathway for NHS Continuing Healthcare
A person with a rapidly deteriorating condition where the condition may be entering a terminal phase, can be 'fast tracked' for immediate provision of NHS Continuing Healthcare.
In fast track cases, the Fast Track Pathway Tool replaces the NHS Continuing Healthcare Checklist and DST. However, a Fast Track Pathway Tool can also be completed after a checklist, if it becomes apparent at that point that the Fast Track criteria are met.
The Fast Track Pathway Tool can be used in any setting. This includes but is not limited to the person's own home, a care home, a hospital, extra care, supported living and shared lives.
In fast track cases, an 'appropriate clinician' determines that the person has a primary health need and makes a recommendation to the ICB.
An 'appropriate clinician' is defined as an individual who is:
- Responsible for the diagnosis, treatment or care of the person under the 2006 Act in respect of whom a Fast Track Pathway Tool is being completed; and
- A registered nurse or a registered medical practitioner.
Others, who are not clinicians as defined above, but involved in supporting those with end of life needs, (including those in wider voluntary and independent sector organisations) may identify the fact that use of the Fast Track Pathway Tool might be appropriate. As such, if you feel that this is the case, you should contact the clinician who is responsible for the diagnosis, care or treatment of the person and ask for consideration to be given to completion of the Fast Track Pathway Tool.
If found eligible for NHS Continuing Healthcare, the ICB should respond promptly and positively to ensure that care arrangements and funding (from the point of referral) are in place without delay.
Full details of the fast track pathway process can be found in the National Framework for NHS and Continuing Health Care.

